Mental health should be a priority, but taking care of oneself rarely comes at no cost. This is why having solid rehab insurance is a must. Aetna is one of the leaders in insurance services, having been around since 1853, and is active in all 50 states. Aetna drug rehab insurance offers a variety of insurance plans, ensuring clients find the coverage that works best for them.
As a center accepting Aetna rehab coverage, We Level Up California aims to help you by answering questions like Does Aetna cover alcohol rehab and does Aetna cover drug rehab? We will share information on Aetna California rehab coverage, including details on services and coverage levels. Remember that policies might change, and the extent of coverage and services available to you may depend on your particular policy, but you can always contact We Level Up CA for additional information on this topic.

We Level Up California’s network of facilities is experienced in treating individuals with mental health and substance abuse concerns. You can trust that our licensed and accredited therapists and counselors are dedicated to providing the needed care. As Aetna´s trusted partner, we strive to help those in need of substance abuse treatment.
Skip To:
About Aetna Rehab Insurance
Aetna is a market leader in health insurance. Its mental health network includes 1.2 million healthcare professionals, almost 700,000 primary care doctors and specialists, and over 5,700 hospitals. Aetna rehab coverage plans, including regular, dental, and vision insurance, have more than 46 million members. As part of the Affordable Care Act (ACA), California drug rehab insurance Aetna covers some or all of the costs of mental health and substance abuse rehab programs, depending on your policy.
Aetna recognizes the significance of mental health and includes mental health care coverage in its products. It will assist in covering the costs of mental health care, whether you have an individual plan, a group plan, coverage through Medicare or Medicaid, or any other type of insurance.
Aetna Alcohol Rehab Coverage and California Drug Rehab Insurance
Knowing how important it is to deal with addiction, Aetna offers Aetna alcohol rehab coverage and California drug rehab insurance Aetna, covering different levels of drug and alcohol rehab treatment. As everyone’s path to recovery from drug and alcohol abuse is different, instead of limiting access to substance abuse treatment, Aetna works closely with each person to find a solution that fits their needs. Aetna tries to be a reliable partner for people recovering from drug and alcohol abuse.
Mental health problems and substance abuse often go hand in hand. Thus, Aetna’s mental health coverage includes treatment benefits for addiction and mental health disorders that occur simultaneously.

Substance Abuse and Mental Health Treatment Services Covered by Aetna California Rehab Coverage
Depending on the challenges you are facing, whether a substance abuse problem or a mental health disorder, you can expect to be offered different levels of care and different types of treatment. Let’s go over the levels of care and types of treatment available to you that your insurance policy may cover.
Get Help. Get Better. Get Your Life Back.
Searching for an Accredited Drug and Alcohol Rehab Centers in Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
FREE Addiction Hotline – Call 24/7Levels of Care
Aetna insurance may cover different levels of care for alcohol and drug rehab, such as:
- Detoxification
- Medication-assisted treatment (MAT)
- Inpatient rehabilitation
- Partial hospital treatment
- Intensive outpatient treatment
- Continuing care programs
Detoxification Services
Detoxification is usually the first step in substance abuse treatment, and its aim is to cleanse the body from the substance used, whether drugs or alcohol. The detox starts by stopping the use of the substance, but it is highly advisable not to do it on your own as it comes with many uncomfortable and potentially dangerous withdrawal effects. The best way to go about it is to go through an alcohol detox or a drug detox in California within a certified facility.
Medication-assisted treatment (MAT)
MAT refers to using FDA-approved medications and therapy to help people deal with cravings and withdrawal symptoms. Aetna usually pays for detox programs that are medically supervised to ensure people can safely stop using drugs or alcohol. Your policy may or may not cover MAT. So, it is crucial to contact your provider or our facility to inquire about your coverage and your options.
Inpatient Treatment
During residential or inpatient treatment, like inpatient alcohol rehab, you stay at a particular facility where you get medical care, therapy, and support 24 hours a day, seven days a week. This is the most intense level of care and the most beneficial one, as it allows deep focus on yourself in a safe and peaceful place.
Depending on your policy, Aetna may pay for all or part of the cost of inpatient care. After meeting the plan’s deductible, some insurance plans feature zero percent coinsurance for in-network hospital stays. A copayment per visit may be necessary for some services under other plans.
Aetna rehab coverage for providers outside the network depends on your plan and living location. Some plans may not pay for out-of-network treatment, while others have 30–50% coinsurance. Out-of-network programs often need to be pre-approved, or there will be a fee each time.
Partial Hospitalization Program
Partial hospitalization (PHP) is a type of program in which a client resides at home but commutes to one of the addiction treatment centers in California up to seven days a week. The idea is to decrease the number of days in a facility over time. These programs focus on the individual´s overall treatment, including:
- Psychopharmacological assessment
- Check-ins
- Therapy (group and individual)
- Skill building
Aetna rehab insurance might cover some portion of the costs for PHP, depending on your insurance plan.
Intensive Outpatient Treatment
As with PHP, intensive outpatient treatment does not require prolonged stays in a facility —in this case, less than 24 hours. It is considered one of the most flexible approaches to treating mental health conditions (substance abuse included), as it allows you to continue with your regular work or school obligations.
Not many rehab centers offer outpatient services (We Level Up California does not, for example), so it´s best to consult directly with your insurance agent before opting for them.
The Continuing Care Programs
The continuing care programs put a lot of emphasis on following up with and helping patients. You can attend weekly meetings to talk to others who have been through treatment programs. These meetings help people feel like they are part of a group and give them ongoing support. Sometimes, social events are set up to celebrate accomplishments and recent recoveries. The positive effects of these programs are significant because they help people stay in touch with each other and get help from their community. Reach out to your insurance provider and see if your policy will cover some of these services.

Types of Substance Abuse and Mental Health Treatment
Aetna California rehab coverage supports both those struggling with mental health issues and substance abuse problems. It helps you cover the costs of different treatments, including counseling services and drug rehab in California.
Coverage for counseling services can benefit individuals seeking mental health support. The specific coverage details may vary depending on your insurance plan. Counseling services typically encompass a range of therapeutic approaches, including:
- Individual therapy
- Group therapy
- Couples therapy
- Family therapy
These services address various mental health concerns, such as anxiety, depression, relationship issues, and stress management.
Aetna rehab coverage may include a wide range of services for people who want to get help for substance abuse. Without worrying about money, you can focus on your recovery from addiction.
Aetna has established guidelines for substance abuse treatment coverage. These guidelines typically consider factors such as:
- The severity of the substance abuse
- The individual’s readiness for treatment
- The medical necessity of the proposed treatment plan
Aetna uses evidence-based guidelines to decide if substance abuse treatment is medically necessary and the right choice. When deciding on coverage, they consider the severity of the addiction, an individual assessment, and recommendations from professionals. Some treatment services may need to be pre-approved or undergo a “utilization review.”

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline (855) 695-1160Does Aetna Pay for Rehab? Insurance Plan Details and Variations
As a result of the Patient Protection and Affordable Care Act, Aetna and other insurance providers now have a legal obligation to prioritize mental health and provide coverage for conditions like depression, OCD, and GAD. The ACA mandates that all health insurance plans cover mental health inpatient services, substance use disorder (SUD) treatment, and behavioral health services like psychotherapy and counseling.
Aetna will pay for mental and behavioral health care if you see a doctor in their network. It still offers help to lessen the financial burden of mental health treatment, which may be slightly more expensive than regular checkup visits. The specific copay under Aetna insurance can vary depending on your policy and plan. Copay amounts can be influenced by location, the type of therapy being received, and whether the therapist is in-network or out-of-network.
To determine your therapy copay, review your Aetna rehab coverage policy and rehab coverage, or you can contact their customer service. They can provide accurate information regarding copay amounts for therapy services and guide you in finding therapists within their network who can meet your needs.

Aetna is committed to supporting individuals in accessing mental health services, and understanding your copay requirements will help you plan and budget for therapy sessions effectively.
Specific Aetna Coverage Details
California rehab coverage Aetna has many plans backed up by a national network of providers to help patients in their community. Open-access, Aetna therapy copay-only, and high-deductible plans are available through Aetna rehab insurance. Here is a bit more about them:
- With an open-access plan, you can choose any doctor you want. You don’t need a referral or a primary care doctor.
- After meeting your deductible, all you’ll have to pay for is your Aetna therapy copay with a copay-only plan. Before you reach your deductible, you will have coverage for visits to your primary care physician and generic medications.
- High-deductible plans offer preventive care and primary care coverage through a primary care physician before the deductible is met (with an Aetna therapy copay), as well as the option of a health savings account. For more information about your plan, visit the member website.

Before deciding on a facility, you should find out what percentage of your treatment costs will be covered by insurance and what percentage you will be responsible for paying out of pocket. Your plan can change Aetna rehab coverage details like deductibles, copayments, and limits. You should review your plan’s benefits before deciding on a rehab facility.
Comfortable Facilities & Amenities
High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned California Addiction Center. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline (855) 695-1160Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Aetna Rehab Coverage Costs and Financial Details
The cost of your rehab will vary from person to person and depends on the rehab center, the type of program you go to, and the services you get. Still, no matter which treatment center you choose or what Aetna rehab coverage plan you have, you will probably have to pay some costs out of your pocket.
When seeking mental health or substance abuse services with Aetna California rehab coverage, it is advisable to consider the following:
Aetna has a network of preferred providers, including therapists and counselors, who have agreed to provide services at negotiated rates. Utilizing in-network providers may result in lower out-of-pocket costs for you.
Aetna may also offer coverage for out-of-network counseling services at different rates. It is important to review your plan’s provisions for out-of-network coverage and understand any potential additional costs you may be responsible for, as out-of-network services may incur additional costs. Rehab centers that take insurance with programs outside of Aetna’s network have not been vetted to ensure they provide care that aligns with industry standards.
All Aetna-approved programs meet rigorous standards for care quality and up-to-date practices. Before starting any treatment program, you should find out from your insurance company if pre-certification is necessary. Some Aetna plans may require preauthorization or prior approval for counseling services. This means you may need to obtain approval from Aetna before starting therapy to ensure coverage. Aetna’s pre-certification process aims to ascertain whether the service or program is clinically appropriate for coverage.
Your plan may involve copayments (fixed fees per session), deductibles (amounts you need to pay out-of-pocket before coverage kicks in), or coinsurance (a percentage of the total cost shared between you and Aetna). Review your plan’s details to understand how these factors apply to counseling services.

Does Aetna Cover Rehab? Contact Aetna Directly for More Information
To determine the extent of your Aetna California rehab coverage and the providers included in your network, it is important to review your policy documents or contact Aetna directly. Aetna’s customer service center is open 24 hours a day, seven days a week. It helps people find treatment options and counselors near them.
Keep in mind that although Aetna covers individual mental disorders and substance abuse therapy, the extent of payment is dependent on the patient’s substance rehab, your insurance plan, and the therapist selected. This means that Aetna rehab coverage is conditional on the member’s specific health plan and the facility they choose for treatment.
Reach out to your insurance agent or verify your insurance policy to feel comfortable and safe when choosing your rehab facility.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL (855) 695-1160End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
FAQs on Aetna Drug Rehab Insurance
Does Aetna cover alcohol rehab?
Yes, Aetna provides coverage for alcohol rehab as part of its behavioral health benefits. The extent of the coverage may depend on your specific plan, including the type of treatment required, such as inpatient or outpatient care. It’s advisable to review your policy details or contact Aetna directly to understand the specifics of your coverage.
Does Aetna cover drug rehab?
Aetna does cover drug rehab under its behavioral health benefits. Coverage can include a range of treatments, from inpatient detoxification to outpatient counseling and therapy. The level of coverage and any associated costs will depend on the specifics of your plan. For detailed information, refer to your plan documents or reach out to Aetna’s customer service.
What types of rehab services are typically covered by Aetna?
Aetna drug rehab insurance generally covers various types of rehab services, including inpatient rehabilitation, outpatient programs, detoxification, medication-assisted treatment, and counseling services. The exact services covered can vary by plan, so it is important to check your policy or speak with an Aetna representative.
Are there any prerequisites for rehab coverage under Aetna plans?
Coverage for rehab services under Aetna plans may require prior authorization or a referral from a primary care physician. Additionally, the services must be deemed medically necessary. It’s important to follow the guidelines specified in your plan to ensure coverage.
How can I find an Aetna-approved rehab facility?
Aetna provides a directory of approved rehab facilities on its website. You can search for providers in your area who are in-network. Alternatively, you can contact Aetna’s customer service for assistance in finding a suitable facility. We Level Up California is one of the facilities that accepts Aetna rehab insurance.
Are there any limits on the duration of rehab treatment covered by Aetna?
There may be limits on the duration of rehab treatment covered by Aetna, which can vary based on the plan. Some plans may have specific caps on the number of days or sessions covered. It’s essential to review your plan specifics or contact Aetna for detailed information.
Rely on We Level Up California for Help and Support
If you or a loved one is struggling with mental health or addiction and have Aetna drug rehab insurance, contact We Level Up California for the support and care you need. Our dedicated team is ready to assist you in navigating your treatment options, providing comprehensive programs tailored to your individual needs. Don’t wait any longer to take the first step toward a healthier and brighter future. Reach out to We Level Up California, a trusted Aetna partner, and let us help you on your path to recovery.
Experience Transformative Recovery at the We Level Up California Treatment Center.
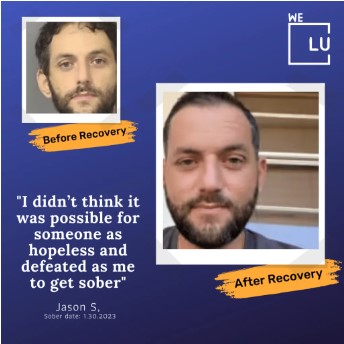
See our authentic success stories. Get inspired. Get the help you deserve.


Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Source
“Mental Health and Substance Abuse Health Coverage Options.” HealthCare.gov, www.healthcare.gov/coverage/mental-health-substance-abuse-coverage. Accessed 25 June 2024.





